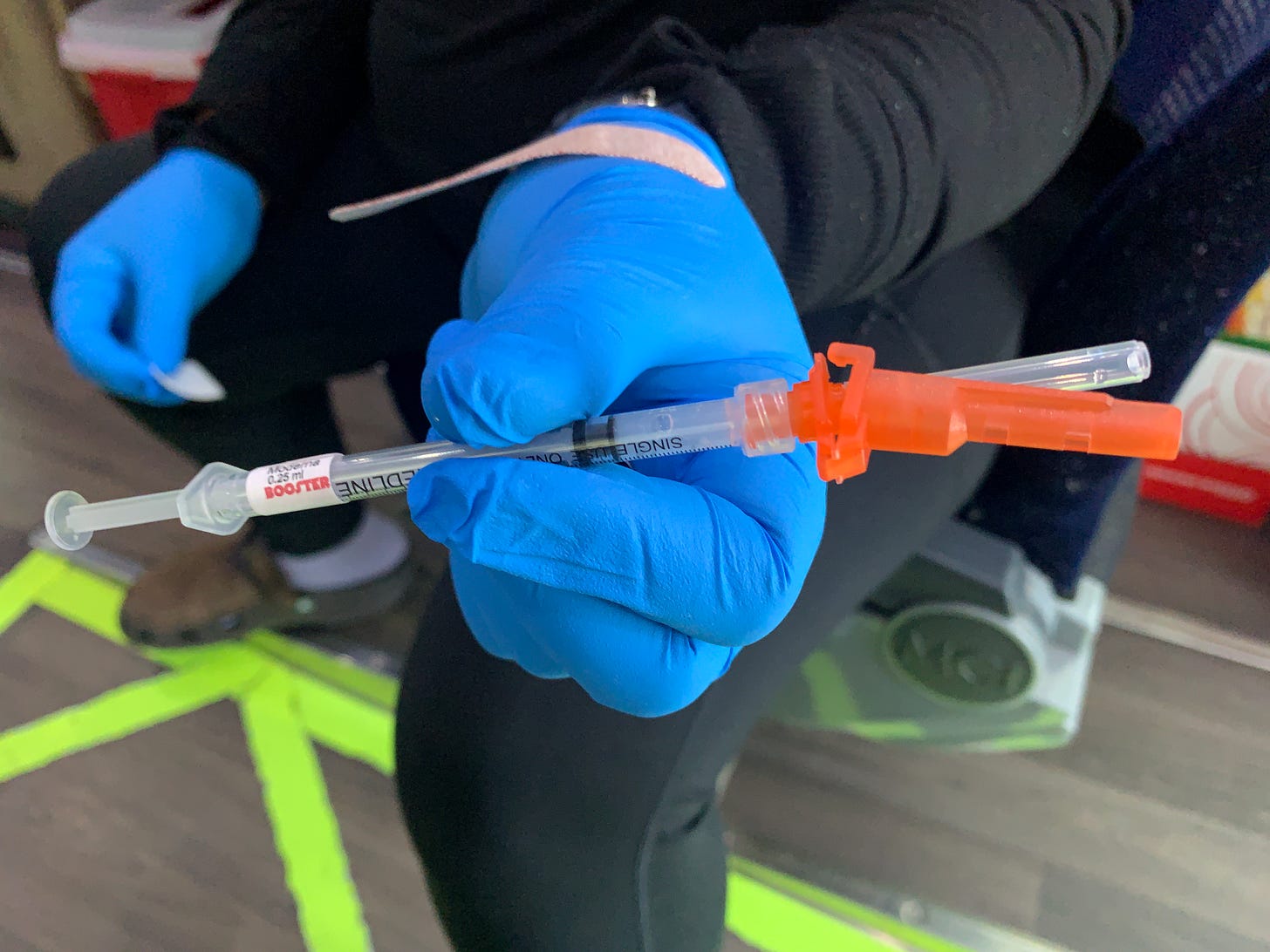
Moderna's patient assistance program promises to cover uninsured and underinsured Americans' vaccination and booster shot costs after May 11, 2023
What could possibly go wrong?
The United States Public Health Emergency ends on May 11, 2023. According Moderna’s press release their “COVID-19 vaccines will continue to be available at no cost for insured people whether they receive them at their doctors’ offices or local pharmacies. For uninsured or underinsured people, Moderna’s patient assistance program* will provide COVID-19 vaccines at no cost. Everyone in the United States will have access to Moderna’s COVID-19 vaccine regardless of their ability to pay.” Doesn’t that sound great?
Before Obamacare expanded Medicaid to low income Americans like me, keeping Crohn’s in remission was spendy, demoralizing, problematic and at points outright humiliating. Three-hundred milligrams every eight weeks thanks my weight hovering around 110 pounds and I only required 300 milligrams every eight weeks.
Since I can’t afford liability insurance yet I’m not going to name the individual insurance policy I had in those pre-Obamacare days but unless you or someone you’re close to has been there it’s really difficult to try and convey how gut wrenching the process of appealing and reapplying legitimate claims when your big name insurer has an incentivized army of claims denial specialists vying for the bonuses they can only obtain by denying the legitimacy of claims submitted by their policy holders.
This happened routinely and at times really messed with sense of reality. I’d get these overdue balances ranging from $500 and $3,000 every other month and have to explain to my dad who was drawing upon his retired government pension to help with my medical expenses. I was also applying for charity care and legal support from a whole slew of outside sources.
And then Remicare, Remicade’s charitable co-pilot came along. Remicare’s process is probably different now than it was back in the aught-teens but like the Moderna it made great copy for a pamphlet or in a press release. It also provided some relief.
I remember filling out form after form. Living in Burbank at the time, its was usually between being on film sets and working odd hours then going from a studio lot to a billing office to make sure nothing got messed up.
The insurance company appeals kept making it seem like they were conceding yet they continued under-reimbursing and justifying everything with clandestine calculations they weren’t obliged to disclose the mechanisms behind.
Why go through all the trouble of reliving this zombie apocalyptic nightmare now?
Because I know what it’s like when that the bureaucratic and financial responsibility falls on the patient, the providers and their billing staff. I know it is unfair and frustrating for everybody yet I did manage throughout all this to stay on Remicade and it’s sugar coated sister charity, Remicare. Both are part of a symbiotic system that benefits the pharmaceutical company.
While I have no doubt that Moderna’s new charity initiative will help fill in some of the gaps that will remain when the US Government pulls out of the COVID vaccine, booster and home test subsidy business on May 11th. Lets hope it isn’t another Afghanistan with right wing science denialist rhetoric and misinformation campaigns filling in. There aren’t many current templates to draw upon to make projections.
“Sponsored patient assistance programs (PAPs) provide access to brand-name medications at little or no cost and have been advocated as a safety net for inadequately insured patients" according to the 2009 Public Health Affairs study that Niteesh Choudhry, Joy Lee, Jessica Agnew-Blais, Colleen Corcoran and William Shrank. Yes the study really is dated 2009 World Health Network pointed me to a study on Patient Assistance Programs that might give a glimpse of some data supporting my concerns.
If l wasn’t working overtime trying to catch up on backlogs while developing what this podcast is going to be like, I could do more digging but for now this will have to suffice. And the data they did manage to obtain is limited.
Of the ones being studied, “Only six programs (4 percent) disclosed how many patients they had directly helped; of those that did disclose the information, estimates ranged from “about six a year” to “more than 14,000 patients in 2006 alone” it was difficult to get a solid grasp on what the outcome of these well intended initiatives actually was when so many companies can opt to withhold information and restrict accountability.
Choudhry et al also called attention to things that resonated with my own frustrating experiences. “The application processes are generally complex, with reading levels greater than those suggested for patients with low health literacy (a problem that is particularly relevant for patients with insufficient insurance coverage).13 Second, instead of supplying patients with medications directly, programs generally give them to patients’ providers, requiring an additional step for patients to obtain them.” People with multiple chronic conditions often had an even more baroque bureaucratic labyrinth to navigate according to the study.
In the best case scenario, Moderna is actively studying Choudhry et al’s findings and subsequent models while looking for new ways to embrace transparency and streamline the process for the underinsured, underinsured and medically vulnerable.
If you have questions, an opinion on why Moderna will or will not get more boosters into arms in 2023, new story ideas or bingo board suggestions please post in the comments.
Immunocompromised Times is a marathon not a sprint. As is the podcast I’m working towards launching by the end of the year. Still trying to catch my breath while catching up on backlogs. Please continue to support my efforts if you can by become a paid subscriber. Paid subscriptions enable me to continue pouring all this time and energy into making immunocompromised centered reporting available to all readers regardless of their ability to pay. And I can actually say that because I control the decision to keep everything in front of —rather than behind— a paywall.




Just stumbled upon this post, and it really hits home! I just battled with a dr's office for over a month to schedule a very overdue infusion for a drug I've taken for over 6 years. The hold up? They require me to get processed by the drug company's copay assistance program...for a $15 copay that I can easily afford (yes, I am 1,000% grateful for my amazing health plan). As a result, I'm significantly overdue for my next dose of medication, wasted hours on phone calls and emails to get this done, and had to reschedule travel plans at my own cost because my infusion landed in the middle of them.
I daydream of a world where insurance+pharma to just provide affordable medications for everyone (vs. complicated pharma assistance programs) and dr offices no longer have to play bottlenecking middlemen.
There never should have to be a whole bunch of unnecessary red tape and bureaucracy for things like this. It's similar with both insurance claims and necessary exemptions to vaccine mandates.